Understanding Venology: An Introduction
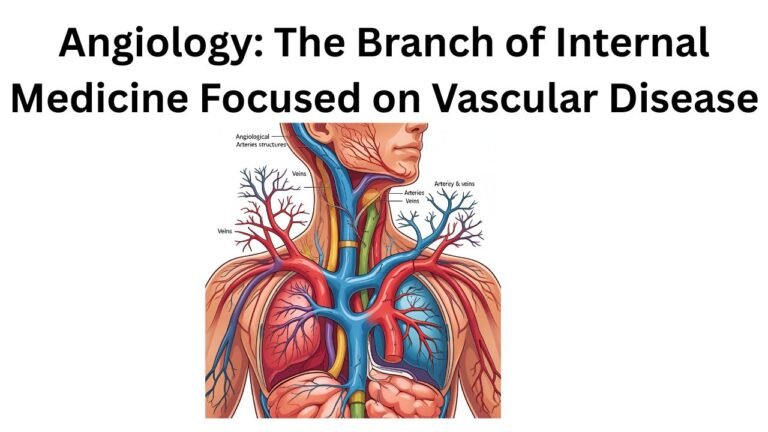
Venology is a specialized branch of medical science and anatomy dedicated to the comprehensive study of veins and their structure, function, and disorders. It plays a pivotal role in understanding the circulatory system, as veins are integral components responsible for returning deoxygenated blood from various parts of the body back to the heart. Unlike arteries, which carry oxygen-rich blood away from the heart, veins are crucial for maintaining overall hemodynamic balance and ensuring efficient blood circulation.
The distinct focus on veins differentiates venology from phlebology, which specifically addresses venous diseases and disorders. While both fields overlap significantly, venology extends beyond pathology to explore the anatomy, physiology, and various functional aspects of veins. This distinct emphasis allows for a broader understanding of venous health, function, and their interactions with other systems within the body.
The historical evolution of venology can be traced back to ancient civilizations where basic knowledge of vein anatomy was recorded. Early medical practitioners laid the groundwork for understanding venous function, albeit with limited technology and theories. Over the centuries, advances in anatomical research and medical technology have significantly expanded our comprehension of the venous system. This evolution has led to the development of innovative diagnostic tools and therapeutic techniques that enhance our ability to address venous diseases effectively.
Today, the study of venology encompasses a wide range of disciplines, including surgical techniques for vein removal, imaging technologies for diagnosing venous pathologies, and research into genetic factors influencing venous diseases. As our understanding of the venous system continues to evolve, so does the importance of venology in medical education and clinical practice, ensuring a more profound comprehension of vascular health and associated conditions.
The Anatomy of Veins
Veins are vital components of the circulatory system, responsible for returning deoxygenated blood from various parts of the body back to the heart. Unlike arteries, which carry oxygen-rich blood away from the heart, veins possess distinct anatomical features that facilitate their unique role. The structure of veins consists of three main layers: the tunica intima, tunica media, and tunica externa.
The innermost layer, the tunica intima, is composed of a thin lining of endothelial cells that create a smooth surface for blood flow. This layer plays a crucial role in reducing turbulence and ensuring efficient circulation. Surrounding the tunica intima is the tunica media, which is thinner in veins than in arteries. This middle layer is primarily made up of smooth muscle and connective tissue, allowing veins to be more flexible and capable of accommodating varying volumes of blood. The outermost layer, the tunica externa, consists of connective tissue that provides structural support and stability to the vein.
One significant characteristic of veins is the presence of valves, which are not found in arteries. These one-way valves ensure that blood flows in the correct direction toward the heart, preventing any backflow that could compromise circulation. This feature is particularly important in the limbs, where blood must travel against gravity to return to the heart. As a result, veins rely on surrounding skeletal muscles to aid in venous return during physical activity.
In summary, the anatomical structure of veins, with their three layers and incorporation of valves, is tailored to facilitate effective blood circulation back to the heart. Understanding these features is essential in the broader context of vascular health, as any disruption in their function can lead to various medical conditions, underscoring the importance of studying venology.
Physiology of Venous Return
Venous return is a fundamental component of the circulatory system, responsible for the efficient transport of deoxygenated blood back to the heart. The physiological mechanisms underlying this process are multifaceted and involve various physiological actions and conditions that facilitate the movement of blood through the veins. One of the primary factors contributing to venous return is the muscle pump action, which plays a vital role during physical activities. As skeletal muscles contract, they exert pressure on the adjacent veins, effectively pushing blood toward the heart. This action is especially pronounced in the lower limbs, where leg movements during walking or exercising promote venous blood flow.
Additionally, respiratory movements significantly impact venous return. During inhalation, the diaphragm descends, creating a negative pressure in the thoracic cavity. This negative pressure not only facilitates the inflow of air into the lungs but also aids in drawing blood back into the heart from the veins. The concurrent actions of the respiratory system and the circulatory system highlight the interdependence of bodily functions, emphasizing how breathing patterns directly affect the efficiency of venous return.
Venous pressure also plays a critical role in this process. The pressure within the veins is usually lower compared to the arterial system, yet it is essential for maintaining adequate blood flow. Several factors, including blood volume and compliance of the veins, influence venous pressure. When there is an increase in blood volume, venous pressure rises accordingly, promoting improved venous return. Furthermore, the presence of venous valves prevents the backflow of blood, ensuring that it ascends towards the heart effectively despite the gravitational forces acting against it.
These physiological mechanisms—muscle pump action, respiratory movements, and venous pressure—all contribute to the intricate process of venous return, highlighting its significance in ensuring effective circulation throughout the body.
Common Venous Disorders
Venous disorders are a significant concern in the realm of vascular health, affecting a considerable portion of the population. Among these disorders, varicose veins, deep vein thrombosis (DVT), and chronic venous insufficiency (CVI) are among the most commonly encountered conditions. Each of these disorders has distinct causes, symptoms, risk factors, and potential complications that warrant thorough understanding.
Varicose veins manifest as enlarged, twisted veins commonly seen in the legs. They usually develop when the valves in the veins become weak or damaged, hindering proper blood flow. Risk factors include age, obesity, prolonged standing, and genetic predisposition. Symptoms are often mild, featuring aching, heaviness, or itchiness in the affected areas. However, if untreated, varicose veins may lead to complications such as skin ulceration or bleeding.
Deep vein thrombosis is a more severe condition characterized by the formation of blood clots in the deep veins, often in the legs. DVT can occur due to inactivity, recent surgeries, or certain medical conditions that affect blood clotting. Symptoms may include swelling, pain, warmth, and redness in the affected leg, although some individuals may remain asymptomatic. If a clot dislodges and travels to the lungs, it can result in a life-threatening pulmonary embolism.
Chronic venous insufficiency occurs when the valves in the veins fail to function effectively, leading to poor blood return to the heart. Risk factors include prolonged standing, obesity, and a history of blood clots. Symptoms may include swelling, aching, and changes in skin color or texture around the ankles and feet. Without appropriate treatment, chronic venous insufficiency can escalate to serious complications, including venous ulcers and significant quality of life impairment.
The prevalence of these venous disorders is notably high, with millions of individuals affected worldwide. Understanding the underlying causes and associated risk factors is crucial for effective management and prevention of these common venous disorders.
Diagnosis of Venous Disorders
The diagnosis of venous disorders is critical for effective management and treatment. Medical professionals utilize a combination of physical examinations and advanced imaging techniques to assess venous health accurately. During a physical examination, healthcare providers look for visible signs of venous problems, such as varicose veins, swelling, discoloration, or skin changes. Additionally, patients may be asked about symptoms like pain, heaviness, or fatigue in the legs, which can indicate underlying conditions.
One of the most common diagnostic tools is ultrasound, particularly Doppler ultrasound, which allows for real-time visualization of blood flow within the veins. This non-invasive test evaluates the structure of the veins and can identify any abnormalities such as clots, valve insufficiency, or restrictions. Doppler ultrasound is favored for its ability to offer immediate results, making it an essential tool in the early detection of venous disorders.
Another important imaging method is venography, which involves injecting a contrast dye into the veins to obtain clear X-ray images. This test provides detailed information about the venous system, helping to identify blockages or abnormalities that may not be visible through ultrasound. While venography is a more invasive procedure, it can be particularly useful in complex cases where other diagnostic methods are inconclusive.
Early diagnosis of venous disorders is essential in preventing severe complications, such as deep vein thrombosis (DVT) or chronic venous insufficiency. By identifying these conditions at an early stage, healthcare providers can recommend appropriate lifestyle changes, medications, or surgical interventions to improve venous health and prevent further issues. Ultimately, utilizing a combination of physical assessment and advanced imaging techniques enhances the diagnosis of venous disorders, facilitating timely and effective treatment strategies.
Treatment Options for Venous Disorders
Venous disorders encompass a variety of conditions affecting the veins, commonly manifested as varicose veins, chronic venous insufficiency, or deep vein thrombosis. Addressing these issues involves a range of treatment options, ranging from conservative management techniques to more invasive clinical interventions and surgical procedures. Each treatment modality is tailored to the specific condition and severity of the venous disorder.
Initially, conservative management is often recommended to alleviate symptoms and improve quality of life. This approach includes lifestyle modifications such as maintaining a healthy weight, engaging in regular physical activity, and elevating the legs to enhance venous return. Additionally, patients may be advised to wear compression stockings, which exert pressure on the legs to promote better circulation and reduce swelling.
When conservative management proves insufficient, clinical interventions may be considered. One of the notable non-surgical options is sclerotherapy, a procedure where a sclerosant solution is injected into the affected veins, causing them to close and redirect blood flow to healthier veins. This method is particularly effective for smaller varicose veins and spider veins, often yielding satisfactory cosmetic results.
Another innovative approach is endovenous laser therapy (EVLT), which utilizes laser energy to close off problematic veins. During this minimally invasive procedure, a catheter is inserted into the affected vein, and laser energy is applied to the vein wall. This results in the vein collapsing and subsequently being absorbed by the body, significantly diminishing the symptoms associated with venous disorders.
In more severe cases, surgical options may become necessary. Traditional surgical interventions include vein stripping or ligation, which involve the removal or tying off of problematic veins. These procedures, while effective, typically require a longer recovery time compared to minimally invasive options. Ultimately, the selection of an appropriate treatment strategy depends on individual patient circumstances, emphasizing the importance of consulting a healthcare professional who specializes in venous disorders for personalized advice and care.
Preventive Measures for Venous Health
Maintaining healthy veins is crucial for overall circulatory well-being and the prevention of venous disorders. One of the primary strategies for promoting good venous health involves incorporating lifestyle modifications that resonate with healthy habits. Regular physical activity is essential; it helps enhance blood circulation, particularly in the lower extremities, thereby preventing vein-related ailments such as varicose veins. Engaging in low-impact exercises, such as walking, cycling, and swimming, can be especially beneficial. It is advisable to exercise for at least 30 minutes most days of the week, as this not only improves vein function but also contributes to weight management, which is vital for venous health.
Moreover, it is important to be mindful of prolonged sitting or standing, as these positions can impede blood flow and increase the risk of venous disorders. To combat this, consider taking regular breaks during sedentary activities, such as standing or walking around every 30 minutes. Elevating the legs periodically can also assist in reducing pressure on the veins.
Diet plays a significant role in venous health as well. Consuming a balanced diet rich in fiber, fruits, and vegetables can help prevent constipation, which may exert strain on the veins. Additionally, incorporating foods high in flavonoids—such as berries, citrus fruits, carrots, and dark chocolate—can enhance circulation and support vein strength. It is also wise to stay well-hydrated, as this aids in maintaining optimal blood viscosity.
In conclusion, adopting these preventive measures can significantly reduce the risk of developing venous disorders. By focusing on a combination of regular exercise, conscious movement practices, and a nutritious diet, individuals can foster better venous health and contribute to their overall well-being. Implementing these lifestyle changes is a proactive step towards preventing potential venous complications in the future.
The Role of Research in Venology
Research plays a pivotal role in advancing venology, the specialized study of veins and venous disorders. As the medical field continually evolves, innovative studies are being conducted to enhance our understanding of venous health and disease. Recent research has focused on the underlying mechanisms of various venous conditions, such as chronic venous insufficiency and venous thromboembolism. By unraveling the complex interactions within the venous system, researchers aim to identify new therapeutic targets that could significantly improve treatment outcomes.
Moreover, advancements in imaging technology and molecular biology are paving the way for more precise diagnostic tools. For instance, non-invasive imaging techniques, such as ultrasound and magnetic resonance venography (MRV), have transformed how venous diseases are diagnosed. These innovations not only allow for earlier detection but also enable clinicians to monitor disease progression over time effectively. By utilizing these advanced techniques, healthcare providers can develop personalized treatment plans that cater to the specific needs of each patient.
In addition to diagnostic improvements, research is being directed toward innovative treatment methods for venous disorders. Minimally invasive procedures, such as endovenous laser therapy and radiofrequency ablation, have emerged as effective alternatives to traditional surgical approaches. Ongoing clinical trials are examining the long-term efficacy and safety of these new interventions, designed to alleviate symptoms and prevent complications associated with venous diseases.
Looking ahead, the future of venous research appears promising. As awareness of venous health continues to grow, significant funding and collaboration between researchers and clinical practitioners will likely foster new insights and interventions. By prioritizing research in venology, the medical community can enhance patient care, improve quality of life, and ultimately reduce the burden of venous diseases on individuals and healthcare systems alike.
Conclusion: The Significance of Venology
Venology, the specialized study of veins, plays a crucial role in the field of medicine and public health. The intricate network of veins in the human body is essential for maintaining proper circulation and overall health. Veins facilitate the return of deoxygenated blood to the heart, and any abnormalities or diseases within this system can have far-reaching consequences on an individual’s well-being. As awareness regarding venous health grows, it becomes increasingly clear that understanding and monitoring venous conditions is vital for early diagnosis and effective treatment.
One significant aspect of venology is its influence on the prevention and management of various health issues. Venous diseases, such as chronic venous insufficiency and deep vein thrombosis, can lead to serious complications if left untreated. Educating the public about the signs and symptoms of venous disorders is essential to promote timely medical intervention. Furthermore, exploring the risk factors associated with venous diseases, including lifestyle choices such as physical inactivity and obesity, can empower individuals to adopt healthier habits that contribute to better venous health.
Another vital consideration is the need for more research in venology. As the global population continues to age, the prevalence of venous disorders is likely to rise, necessitating an enhanced focus on this field. Increased investment in venology research can uncover innovative treatments and improve patient outcomes. Additionally, it is imperative to integrate venous health education into medical training programs to ensure that healthcare professionals are well-equipped to recognize and address veinal issues. By fostering a greater understanding of venology and advocating for its significance, we can collectively contribute to better health outcomes and enhance the quality of life for those affected by venous disorders.